An ectopic pregnancy occurs when a fertilized egg implants and grows outside the uterus, most often in a fallopian tube. Since the fallopian tubes cannot support a growing embryo, the condition can cause internal bleeding and become life-threatening without prompt medical treatment. Understanding the risk factors helps in early detection and prevention.
1. Previous Ectopic Pregnancy
Women who have had an ectopic pregnancy before are at a higher risk of recurrence. The earlier condition might have caused scarring or structural damage to the fallopian tubes, affecting the normal passage of eggs in future pregnancies.
2. Pelvic Inflammatory Disease (PID)
PID, often resulting from untreated sexually transmitted infections (like chlamydia or gonorrhea), can damage the lining of the fallopian tubes. This damage may prevent the fertilized egg from reaching the uterus, leading to implantation within the tube.
3. Previous Pelvic or Abdominal Surgery
Surgeries on the uterus, ovaries, or fallopian tubes — including procedures for tubal ligation, reversal, or cyst removal — can cause scar tissue or adhesions. These adhesions can block or narrow the tubes, increasing the chance of an ectopic pregnancy.
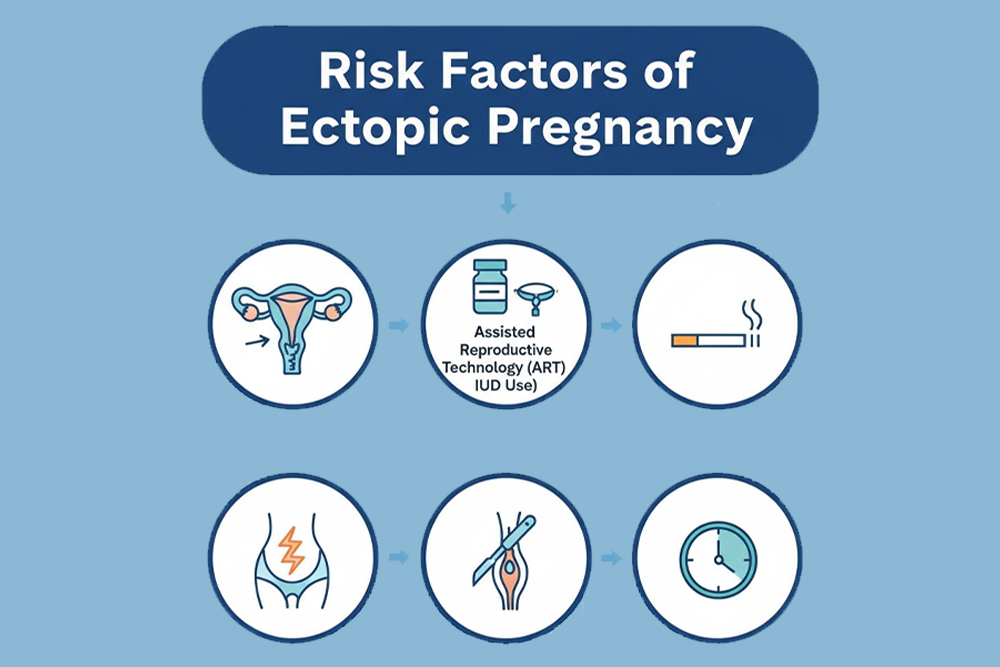
4. Fertility Treatments and Assisted Reproductive Techniques (ART)
Procedures such as IVF, ICSI, or ovulation induction can increase the risk slightly. This is due to altered egg movement or multiple embryos being placed near the tubes during treatment. However, regular monitoring during fertility care minimizes the risk.
5. Use of Intrauterine Devices (IUDs)
Pregnancy with an IUD in place is rare, but when it occurs, it has a higher chance of being ectopic. The IUD prevents uterine implantation, so the fertilized egg may implant in the tube instead.
6. Smoking
Cigarette smoking affects the cilia (tiny hair-like structures) inside the fallopian tubes that help move the egg toward the uterus. The toxins in tobacco slow down or damage these cilia, leading to a higher risk of tubal implantation.
7. Age and Reproductive Factors
Women aged 35 years or older face a slightly increased risk due to age-related tubal changes. Conditions like endometriosis, congenital tubal abnormalities, or fibroids that alter normal reproductive anatomy can also contribute.
8. Hormonal and Infertility-Related Issues
Hormonal imbalances affecting ovulation, tubal motility, or uterine lining can disrupt the normal travel of the egg. Similarly, women with a history of infertility may have underlying structural or functional issues that predispose them to ectopic pregnancies.
9. Family History and Genetic Factors
A family history of ectopic pregnancy may also raise an individual’s risk, suggesting possible genetic or anatomical predispositions.
10. Lack of Early Prenatal Care
Unrecognized or delayed diagnosis is another major factor. Women who miss early prenatal checkups may not detect ectopic symptoms in time, leading to complications.
Early Symptoms to Watch For
- Missed period and positive pregnancy test
- Sharp or stabbing abdominal or pelvic pain
- Vaginal bleeding or spotting
- Shoulder pain (due to internal bleeding) during urination
- Dizziness or fainting
If any of these symptoms occur — especially with a positive pregnancy test —immediate medical attention is essential